The orthopedic surgeon, former congressman, and 23rd Secretary of Health and Human Services discusses the role of private equity in healthcare, clinical autonomy, and site-neutral payments.
Levin Associates spoke with Dr. Tom Price at the 6th annual Physician Transactions Conference in Las Vegas in March 2023. This Q&A has been lightly edited for clarity and brevity.
I’m curious to get your take on the role of private investment in healthcare, considering your background in both medicine and policy.
What private equity brings to the table, if you have the right partner, is capital, resources, talent, and expertise on the operations side. The best private equity platforms that are partnering with practices are the ones that say, “Doc, you go practice. Do whatever you do. You know exactly how to do it. We don’t know anything about that. We will assume the responsibility for the operations side and work with you to determine how the practice grows.”
Those are things that any physician worries about because they know that they don’t have any training in operations and they don’t have training in business development. Private equity fills voids that exist in the physician’s experience.
I used to joke that when I got my medical degree, I walked across the stage and they handed me my diploma, and then they whispered in my ear, “Oh, by the way, you get to run a business too, without any training.” That’s essentially what it was.
It’s different now. For many doctors coming out of medical school now and going into residency, their preferred practice setting is as employed physicians. They recognize their shortcomings from a business standpoint and so they’re happy to be an employee.
What they will discover and have discovered in many instances is that the entities that are employing them oftentimes won’t allow them to have clinical autonomy, which is where private equity comes in.
Why wouldn’t they have clinical autonomy as an employed physician?
Hospitals provide a wonderful service. But how they reach an appropriate bottom line, from their perspective, is to become as efficient as possible and standardize the care. But the standardized way may or may not be what the doctor believes is most appropriate for each patient. That’s where the rub comes for orthopedists.
Aren’t the big private equity companies focused on the bottom line?
There are good guys and gals out there and there are bad guys and gals out there in everything. And private equity is no different. I’m biased because I work with Triumph Orthopedics and Shore Capital Partners and what they bring to the table, I believe, is a recognition that good medicine makes good business.
Throughout my career practicing orthopedics and serving in the public sector, one of my principles has been to ensure that patients and families and doctors are the ones making the medical decisions, and nobody else. Insurance companies, hospital administrators, and businesses ought not to be making medical decisions. It needs to be doctors and patients. And if you ask patients who they want to help them make medical decisions, it’s their doctor.
When I left Washington, D.C., I didn’t want to lobby and I didn’t want to go back and practice orthopedics again. I was told that I ought to look at private equity but I was skeptical. I said, “I don’t want to look at private equity. Goodness, gracious, those aren’t the good guys.”
But then I met with a number of different companies, and Shore was the one that convinced me that they were committed to the idea that good medicine makes good business, and committed to allowing the physician to continue their autonomy and their practice.
I’ve never been in a discussion with anybody at Triumph or at Shore where they said, “We need to change how this doctor practices.” It doesn’t even come up. It’s not even a discussion because they’re focused on, “How do we improve operations? How do we grow the business?” And that’s what doctors want as well.
What do physicians need to keep in mind when they’re considering partnering with private equity?
If I were still practicing and a private equity company knocked on my door and said “Hey, we’d love for you to join us,” there are two big questions that I would ask.
One is, “Are you going to tell me how to practice medicine?” If the answer to that is “maybe,” “we don’t know,” or “yes,” then I don’t want anything to do with them. The answer to that question has to be “no” from the very beginning.
The second is, “What does this mean financially for me and my family?” Most orthopedic surgeons are doing relatively well so they want to know how private equity is going to ensure that that continues, without harming their ability to practice medicine the way they believe that they ought to.
Partnering with private equity is an opportunity for doctors to monetize the sweat equity they’ve put into their practice. The doctors are able to gain greater financial security by having equity/ownership in the new business entity, resulting in a potentially rewarding investment not currently available to them in their independent practice.
What would you say to patients who may feel concerned about whether private equity will impact the quality of care, or raise costs?
No physician wakes up in the morning and says, “I hope I do a bad job today.” They want to do a great job on every single patient.
From a patient standpoint, they ought not to see any difference other than the ability of their doctor to be able to care for them more effectively, more efficiently, and more responsibly, with the highest quality care possible.
More procedures can now be performed in outpatient settings. What’s your take on that shift?
Those decisions need to be based on the science and the quality of care that can be provided. Patients should be able to get the highest quality care in the setting that their physician believes is most appropriate.
When I was in the public arena, I was a big supporter of site-neutral payments. Insurance companies or the government should be paying the same amount for a total hip replacement done in a hospital as in an outpatient setting or ambulatory surgery setting. And that oftentimes isn’t the case.
Erin Laviola is a writer for Levin Associates.
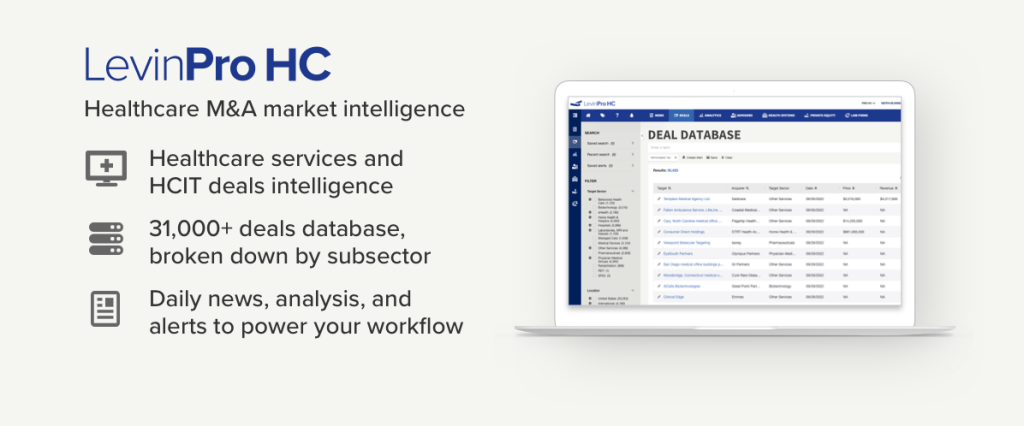
Levin Associates provides comprehensive coverage of the deals, companies, and trends shaping the healthcare industry. Clients access proprietary M&A transaction data and daily news/analysis through the LevinPro platform. Schedule a demo today to see what LevinPro can do for your team.
© 2023 Irving Levin Associates, LLC. All rights reserved.

